Can You Have Osteoarthritis and Psoriatic Arthritis Together
Feb 17, 2021
Psoriatic Arthritis vs Osteoarthritis: five Important Facts You Should Know
Posted Past: Candice Groves

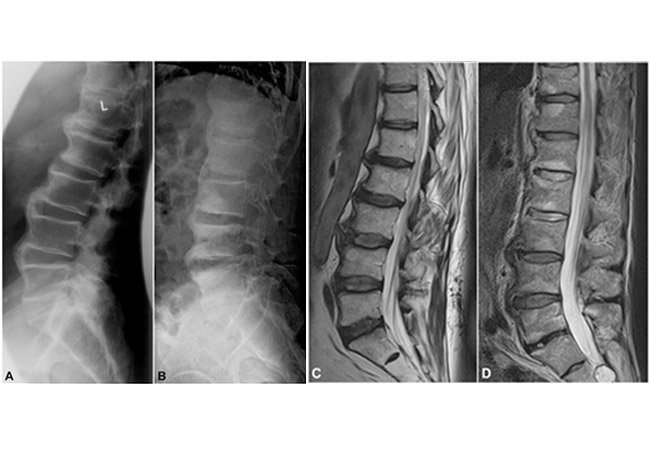
Psoriatic arthritis (PsA) is a chronic autoimmune disease that causes inflammation of the skin and joints. Skin tin go itchy and scaly, and the inflamed joint areas can become stiff, bloated, and painful. It is estimated that as many equally xxx% of people who accept psoriasis volition too develop Psoriatic arthritis. Nevertheless, as it is sometimes activated in the articulation area before symptoms appear on the peel's surface, people can fault it for osteoarthritis (OA) since both forms of arthritis display shared symptoms of articulation hurting, swelling, stiffness, and reduced flexibility. In this commodity, we volition be looking at psoriatic arthritis vs osteoarthritis radiology, causes and symptoms, and other facts yous should know about the two forms of arthritis.
What'due south the difference Between OA and PsA?
The difference is that osteoarthritis is non an autoimmune disease similar PsA but is a class of degenerative joint disease promoted by the wear and tear of cartilage and basic rubbing together. Similar to psoriatic arthritis, OA exhibits the inflammation and pain symptoms mentioned above, and in serious cases or without proper self-management, information technology can immobilize people.
Psoriatic arthritis (PsA) and osteoarthritis (OA) are the two most mutual forms of arthritis. Osteoarthritis is a consistent condition, whereas PsA can flare upward irregularly. Other unique symptoms associated with OA include grinding and clicking of the articulation area during movement, distorted articulation shape, and difficult lumps of bone growth near the joint. Symptoms specific to PsA include a red rash and silvery-white patches on the skin, smash pitting, swollen fingers and toes, centre redness and pain, tendon and ligament pain, and fatigue.
Is Psoriatic Arthritis Worse than Osteoarthritis?
The progress of your PsA or OA determines the severity and whether one or the other is worse. Some cases of PsA are mild, and since flares can come up and get, it may not interfere with a person's life as much as the constant OA tin. Severe cases of osteoarthritis tin create daily discomfort and pain. Both require proper cocky-management to mitigate pain and wearisome the progression of the diseases. If conditions are misdiagnosed or treated inappropriately, information technology tin have a debilitating effect on the person suffering from arthritis.
Can y'all take Psoriatic Arthritis and Osteoarthritis at the Aforementioned Time?
The risk for OA in patients with PsA is significantly higher than for those who exercise not suffer from the condition, with the prevalence of OA being 22.1% in the PsA group. This overlap tin prove difficult when identifying and ten-raying psoriatic arthritis and osteoarthritis. An incorrect diagnosis tin can lead to the wrong treatment of medication and therapy, and as a consequence, the condition worsens. Looking out for symptoms unique to each condition, in addition to radiology procedures, go paw in hand to ensure an accurate diagnosis.
5 Facts You Should know almost Psoriatic Arthritis vs Osteoarthritis
To summarize the causes and symptoms of both Psoriatic Arthritis and Osteoarthritis, here are v important facts to know.
i. PsA Causes
Psoriatic Arthritis doesn't have ane articulate determiner which triggers the affliction; withal, the post-obit gamble factors tin can promote PsA;
- • Psoriasis: more than eight million people take psoriasis in the U.S.
- • Allowed abnormalities, i.due east., higher levels of certain proteins in the blood such as cytokines, which trigger inflammation.
- • Environmental factors: such equally a bacterial or viral infection and physical trauma.
- • Genetics: approximately 40% of people with psoriasis or psoriatic arthritis accept family members with psoriasis or psoriatic arthritis.
two. OA Causes
Osteoarthritis is a outcome of the wear and tear when the cartilage that supports the basic in your joints progressively deteriorates. The following factors tin can increment the chance of OA;
- • Genetics and Gender: Studies have shown that the influence of genetic factors is between 39% and 65% in radiographic OA of the mitt and knee in women, effectually sixty% in OA of the hip, and approximately 70% in OA of the spine. Women are also more than likely to become OA.
- • Obesity: Weight adds pressure level to your joints, which ultimately wears the cartilage down and once the bone is painfully rubbing against os, it can become a astringent problem.
- • Joint Injury or malformation: if joints take been damaged or haven't formed ordinarily, there is an increased run a risk of having OA.
- • Age: the risk of getting OA increases every bit yous get older, particularly over the historic period of fifty.
3. PsA Symptoms and Treatments
Symptoms of PsA can include the following;
- • A red rash and/or silverish-white patches on the pare
- • Smash pitting
- • Swollen fingers and toes
- • Middle redness and pain
- • Tendon and ligament pain
- • Fatigue
Some of the mutual treatments of PsA include;
- • Topical treatments for peel and smash irritations
- • Medication and steroid injections to reduce inflammation and hurting
- • Joint replacement surgery for severe cases
iv. OA Symptoms and Treatments
Symptoms of OA can include the post-obit;
- • Grinding and clicking of the joint area when moving
- • Hurting and stiffness of joints afflicted
- • Inflammation
- • Decreased flexibility and immobility
Some of the treatments available to those with OA to reduce inflammation, relieve pain, meliorate mobility, and dull progression include;
- • An exercise program to lose weight to decrease pressure on joints
- • A modified diet to reduce intake of inflammation-inducing foods and to maintain a salubrious weight
- • Medication and supplements
- • Therapies such as acupuncture and exercises to strengthen areas with OA
- • Invasive treatments such every bit a joint replacement for severe cases or cortisone injections.
5. Management of PsA and OA
Equally each person experiences individual symptoms, the many different options available in terms of treatment and management of psoriatic arthritis and osteoarthritis may not be suitable for your specific needs. Information technology is always best to get communication from professionals and learn how to cocky-manage your arthritis with support from personalized programs and communities dealing with the same condition. Keeping connected with your loved ones is important, as arthritis can take a price on your mental wellbeing.

Terminal Thoughts
With two of the virtually common forms of arthritis having the potential to overlap, you must ensure that whether you are currently experiencing psoriatic arthritis or osteoarthritis, you have a clear diagnosis and treat each condition individually to alleviate the symptoms of both and to maintain mobility. If you are experiencing any of the shared symptoms of joint pain, swelling, stiffness, and reduced flexibility just do not show whatsoever signs on the peel, it is all-time to consult with a doctor for a clinical diagnosis. When you empathize the underlying condition, you tin proactively self-manage and live a normal life.
leworthyyouslorou.blogspot.com
Source: https://www.myarthritisrx.com/blog/2021/02/17/psoriatic-arthritis-vs-osteoarthritis
0 Response to "Can You Have Osteoarthritis and Psoriatic Arthritis Together"
Post a Comment